respiratory system assessment pdf
Respiratory system assessment is a critical component of clinical practice‚ aiding in the diagnosis and management of respiratory disorders․ It combines patient history‚ physical examination‚ and diagnostic tests to evaluate lung function and overall respiratory health‚ ensuring accurate and effective care․
1․1 Importance of Respiratory Assessment
Respiratory assessment is vital for early detection of lung disorders‚ monitoring disease progression‚ and guiding treatment plans․ It helps identify abnormalities‚ such as asthma‚ COPD‚ or infections‚ ensuring timely interventions․ Accurate assessment improves patient outcomes by enabling personalized care and preventing complications․ Regular evaluations also enhance understanding of respiratory health‚ facilitating better management of chronic conditions and promoting overall well-being․ It is a cornerstone of pulmonary care‚ essential for both diagnosis and long-term disease management․
1․2 Objectives of Respiratory System Evaluation
The primary objectives of respiratory system evaluation are to identify respiratory disorders‚ assess symptom severity‚ monitor disease progression‚ evaluate treatment effectiveness‚ and improve patient outcomes․ It aims to systematically collect data on lung function‚ detect abnormalities‚ and guide personalized care plans‚ ensuring accurate diagnosis and optimal management of respiratory health․
Components of Respiratory Assessment
Respiratory assessment involves a comprehensive evaluation of patient history‚ physical examination‚ and diagnostic tests to accurately identify and manage respiratory conditions‚ ensuring effective patient care and outcomes․
2․1 Patient History and Symptom Review
A thorough patient history and symptom review is the cornerstone of respiratory assessment․ It involves gathering information about the patient’s medical history‚ current symptoms‚ and lifestyle factors․ Key elements include respiratory symptoms (e․g․‚ cough‚ dyspnea)‚ duration‚ severity‚ and associated factors․ Past medical history‚ medications‚ allergies‚ and environmental or occupational exposures are also essential․ This step helps identify patterns‚ risk factors‚ and potential causes of respiratory issues‚ guiding further evaluation and diagnosis․ Accurate documentation ensures a comprehensive approach to patient care․
2․2 Physical Examination Techniques
Physical examination techniques in respiratory assessment include inspection for chest deformities or abnormal breathing patterns‚ palpation to detect vibrations or tenderness‚ and percussion to assess lung density․ Auscultation is performed to evaluate breath sounds‚ identifying abnormalities like wheezes‚ crackles‚ or pleural rubs․ These methods provide crucial insights into respiratory function and help identify potential pathologies‚ guiding further diagnostic steps and management strategies․
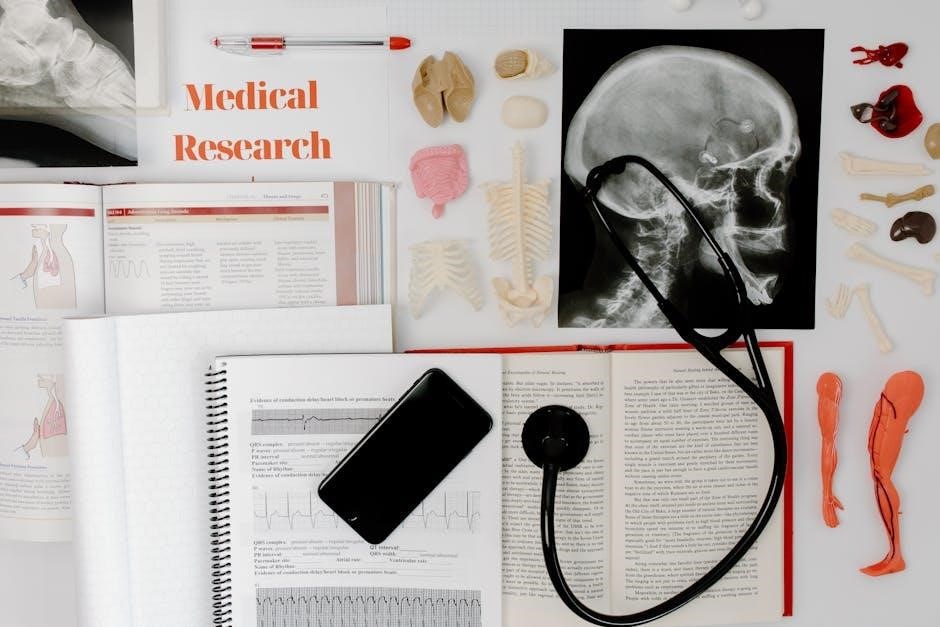
2․3 Diagnostic Tests and Tools
Diagnostic tests are essential for accurately assessing respiratory health․ Common tools include spirometry‚ peak flow meters‚ and pulse oximetry․ Imaging techniques like X-rays and CT scans provide visual insights․ Blood gas analysis measures oxygen and carbon dioxide levels‚ while pulmonary function tests (PFTs) evaluate lung capacity and airflow․ These tools help identify abnormalities‚ monitor disease progression‚ and guide treatment plans‚ ensuring comprehensive respiratory care․
Subjective Assessment
Subjective assessment involves gathering patient-reported information to understand respiratory health․ It includes symptoms‚ medical history‚ and lifestyle factors to guide further evaluation and personalized care plans effectively․
3․1 Identifying Respiratory Symptoms
Identifying respiratory symptoms is the first step in subjective assessment․ Common symptoms include coughing‚ dyspnea‚ wheezing‚ chest pain‚ and sputum production․ Patients may report fatigue‚ fever‚ or weight loss․ These symptoms help differentiate between acute and chronic conditions‚ guiding further evaluation․ A detailed history ensures accurate diagnosis and appropriate management․ Understanding the onset‚ duration‚ and severity of symptoms is crucial for developing a comprehensive care plan․
3․2 Review of Medical History
A thorough review of the patient’s medical history is essential to identify potential respiratory risk factors‚ such as pre-existing conditions‚ allergies‚ or previous surgeries․ This step helps uncover chronic diseases like asthma or COPD‚ which may impact current symptoms․ Past infections‚ smoking history‚ and occupational exposures are also critical to assess․ Understanding the patient’s medical background provides context for symptoms and aids in differential diagnosis‚ ensuring a comprehensive approach to respiratory care and management․
3․3 Lifestyle and Environmental Factors
Lifestyle and environmental factors significantly impact respiratory health․ Smoking‚ exposure to pollutants‚ occupational hazards‚ and poor air quality can contribute to respiratory conditions․ Assessing these factors helps identify risks‚ such as secondhand smoke or radon exposure‚ and informs preventive measures․ Understanding a patient’s lifestyle‚ including exercise habits and substance use‚ provides insights into overall respiratory well-being․ Environmental factors like mold‚ pet dander‚ or pollution exacerbate conditions like asthma or COPD․ Addressing these elements is crucial for targeted interventions and improved outcomes․

Objective Assessment
Objective assessment involves physical examination techniques such as inspection‚ palpation‚ percussion‚ and auscultation to evaluate respiratory function and identify abnormalities․
4․1 Inspection and Observation
Inspection and observation are the initial steps in respiratory assessment‚ focusing on visible signs of respiratory distress or abnormalities․ Key observations include breathing patterns‚ use of accessory muscles‚ chest symmetry‚ and visible deformities or injuries․ Assess posture‚ cyanosis‚ clubbing‚ or edema‚ which may indicate underlying conditions․ Note the presence of oxygen therapy‚ tracheostomy‚ or other respiratory devices․ These visual cues provide critical insights into the patient’s respiratory status‚ guiding further evaluation and informing diagnostic decisions․
4․2 Palpation and Percussion
Palpation and percussion are essential techniques in respiratory assessment․ Palpation involves examining the chest for tenderness‚ masses‚ or vibrations‚ while percussion uses tapping to evaluate lung density․ These methods help identify abnormalities such as hyperresonance (indicative of air trapping) or dullness (suggesting fluid or consolidation)․ They provide valuable insights into underlying conditions like pneumonia or pleural effusion‚ guiding further diagnostic steps and informing clinical decision-making․ Proper technique ensures accurate findings‚ enhancing the overall assessment process․
4․3 Auscultation of Breath Sounds
Auscultation involves listening to breath sounds using a stethoscope to assess lung function and detect abnormalities․ Normal breath sounds‚ such as vesicular sounds‚ indicate healthy lungs․ Abnormal sounds‚ like crackles‚ wheezes‚ or rhonchi‚ may suggest conditions such as pneumonia‚ asthma‚ or COPD․ This technique is crucial for identifying patterns and localizing pathologies‚ aiding in differential diagnosis and guiding further investigation․ Accurate interpretation of breath sounds is essential for effective respiratory care and management․
Diagnostic Tests in Respiratory Assessment
Diagnostic tests are essential for evaluating respiratory health‚ providing insights into lung function‚ structural abnormalities‚ and gas exchange efficiency․
5․1 Pulmonary Function Tests (PFTs)
Pulmonary Function Tests (PFTs) are essential for evaluating lung function and diagnosing respiratory disorders․ Common tests include spirometry‚ which measures airflow and lung volumes‚ and diffusing capacity for carbon monoxide (DLCO)․ PFTs assess parameters like forced vital capacity (FVC) and forced expiratory volume in one second (FEV1)․ They help identify obstructive or restrictive pulmonary diseases‚ such as asthma or chronic obstructive pulmonary disease (COPD)․ Accurate interpretation of PFT results is critical for clinical decision-making and monitoring treatment effectiveness․
5․2 Chest X-Ray and Imaging Studies
A chest X-ray is a fundamental diagnostic tool in respiratory assessment‚ providing visualization of lung tissue‚ pleura‚ and mediastinum․ It helps identify abnormalities such as pneumonia‚ tumors‚ or effusions․ Advanced imaging techniques like CT scans or MRI offer detailed views of lung structures and are particularly useful for complex conditions․ These imaging studies complement clinical findings and pulmonary function tests‚ aiding in the accurate diagnosis and management of respiratory disorders․ They are essential for assessing lung function and structural abnormalities․
5․3 Blood Gas Analysis
Blood gas analysis measures oxygen (O2)‚ carbon dioxide (CO2)‚ and pH levels in arterial blood‚ providing insights into respiratory function and acid-base balance․ It helps assess ventilation‚ oxygenation‚ and gas exchange efficiency․ Common parameters include PaO2 (partial pressure of oxygen)‚ PaCO2 (partial pressure of carbon dioxide)‚ pH‚ bicarbonate (HCO3-)‚ and oxygen saturation (SaO2)․ Abnormal results may indicate respiratory acidosis‚ alkalosis‚ or hypoxemia‚ guiding treatment decisions․ It is essential for diagnosing conditions like asthma‚ COPD‚ and pulmonary embolism‚ and monitoring critically ill patients․

Normal Respiratory Anatomy and Physiology
The respiratory system includes the nasal cavity‚ pharynx‚ trachea‚ bronchi‚ and alveoli․ Air enters through the nose‚ moves through airways‚ and reaches alveoli for gas exchange․ The diaphragm and intercostal muscles facilitate breathing‚ enabling oxygen diffusion into blood and carbon dioxide removal․ Capillaries surrounding alveoli ensure efficient gas exchange‚ vital for cellular respiration and overall bodily function․
6․1 Structure of the Respiratory System
The respiratory system consists of the upper and lower airways‚ including the nose‚ mouth‚ pharynx‚ larynx‚ trachea‚ bronchi‚ and lungs․ The upper respiratory tract facilitates air entry‚ filtration‚ and humidification‚ while the lower tract enables gas exchange․ The lungs contain bronchioles and alveoli‚ where oxygen and carbon dioxide exchange occurs․ The diaphragm and intercostal muscles play a crucial role in breathing mechanics‚ enabling the expansion and contraction of the chest cavity to facilitate airflow․
6․2 Mechanism of Breathing
The mechanism of breathing involves the coordinated contraction and relaxation of the diaphragm and intercostal muscles․ During inhalation‚ the diaphragm descends‚ increasing thoracic cavity volume‚ while the rib cage expands‚ allowing air to enter the lungs․ Exhalation occurs passively as the diaphragm relaxes and the chest wall descends‚ expelling air․ This process is regulated by the autonomic nervous system‚ with the brain’s respiratory centers controlling the rhythm and depth of breathing to maintain adequate oxygenation and carbon dioxide removal․
6․3 Gas Exchange Process
The gas exchange process occurs in the alveoli‚ where oxygen diffuses into the bloodstream and carbon dioxide is removed․ This process is facilitated by the thin walls of alveoli and surrounding capillaries․ Oxygen binds to hemoglobin in red blood cells‚ while carbon dioxide is transported back to the lungs for exhalation․ Efficient gas exchange relies on proper ventilation‚ blood flow‚ and the integrity of the alveolar-capillary membrane‚ ensuring adequate oxygenation of tissues and removal of waste gases․

Signs and Symptoms of Respiratory Disorders
Respiratory disorders often present with symptoms such as coughing‚ shortness of breath‚ and chest pain․ Early identification of these signs is crucial for timely diagnosis and intervention․
7․1 Common Respiratory Symptoms
Common respiratory symptoms include cough‚ dyspnea‚ wheezing‚ chest tightness‚ and sputum production․ These symptoms often indicate underlying conditions such as asthma‚ chronic obstructive pulmonary disease (COPD)‚ or infections․ Coughing may be dry or productive‚ while dyspnea can range from mild to severe․ Wheezing suggests airway obstruction‚ and chest tightness may signal bronchospasm․ Accurate documentation of these symptoms aids in diagnosing respiratory disorders and developing effective treatment plans․ Recognizing these symptoms is essential for early detection and proper management of respiratory conditions․
7․2 Red Flags in Respiratory Assessment
Red flags in respiratory assessment are critical indicators of potential life-threatening conditions․ Symptoms such as severe dyspnea‚ chest pain‚ hemoptysis‚ or sudden onset of respiratory distress warrant immediate attention․ Other red flags include significant weight loss‚ recurrent infections‚ or a history of exposure to harmful substances․ These signs may indicate serious underlying conditions like pneumonia‚ pulmonary embolism‚ or malignancy․ Prompt recognition and referral are essential to ensure timely intervention and improve patient outcomes․ Always prioritize these signs during evaluation․

Abnormal Breath Sounds and Their Significance
Abnormal breath sounds‚ such as crackles‚ wheezes‚ and rhonchi‚ indicate respiratory issues like infections‚ obstructions‚ or inflammation․ Their presence aids in diagnosing conditions and guiding treatment plans effectively․
8․1 Types of Abnormal Breath Sounds
Abnormal breath sounds include wheezes‚ crackles‚ rhonchi‚ and pleural rubs․ Wheezes are high-pitched sounds associated with airway obstruction‚ often seen in asthma or COPD․ Crackles are bubbly sounds heard in conditions like pneumonia or pulmonary fibrosis․ Rhonchi are low-pitched sounds indicating secretions or obstruction․ Pleural rubs are creaking sounds due to inflammation of the pleura․ These sounds help identify underlying respiratory pathologies‚ guiding further diagnostic and therapeutic interventions․
8․2 Clinical Implications of Breath Sound Analysis
Breath sound analysis provides critical insights into respiratory health‚ aiding in the early detection of conditions like asthma‚ COPD‚ or pneumonia․ Abnormal sounds‚ such as wheezes‚ crackles‚ or rhonchi‚ correlate with specific pathologies‚ guiding diagnostic and therapeutic interventions․ Accurate interpretation of these sounds enables clinicians to monitor disease progression‚ assess treatment efficacy‚ and identify complications․ This non-invasive tool enhances patient care by offering timely and actionable information‚ making it a cornerstone of respiratory assessment and management strategies․
Interpretation of Respiratory Assessment Findings
Interpretation involves analyzing symptoms‚ physical exam results‚ and diagnostic data to identify patterns‚ confirm diagnoses‚ and guide treatment planning‚ ensuring comprehensive respiratory care․
9․1 Correlating Symptoms with Physical Exam Results
Correlating symptoms with physical exam findings is essential for accurate diagnosis․ For instance‚ a patient reporting cough and shortness of breath may show wheezing or crackles on auscultation‚ indicating asthma or infection․ This integration helps identify patterns‚ such as pleuritic pain with friction rubs suggesting pleurisy․ It ensures a comprehensive understanding of respiratory issues‚ guiding further investigation and treatment plans․ Accurate correlation enhances clinical decision-making and improves patient outcomes in respiratory care․
9․2 Integrating Diagnostic Test Results
Integrating diagnostic test results involves correlating findings from pulmonary function tests‚ imaging‚ and blood gas analysis to form a comprehensive understanding of respiratory function․ This systematic approach ensures that all data points align with clinical observations‚ enhancing diagnostic accuracy․ By linking symptoms‚ physical exam results‚ and test outcomes‚ healthcare providers can identify patterns and abnormalities‚ guiding further management and treatment plans․ This integration is crucial for developing targeted interventions and improving patient outcomes in respiratory care․
Documentation and Reporting
Accurate documentation of respiratory assessment findings ensures clear communication and continuity of care‚ while comprehensive reporting facilitates informed decision-making and adherence to legal and professional standards․
10․1 Effective Documentation Techniques
Effective documentation in respiratory assessment involves clear‚ concise‚ and organized recording of findings․ Use standardized templates to ensure consistency and completeness․ Include dates‚ times‚ and patient identifiers for accuracy․ Document subjective symptoms‚ objective data‚ and diagnostic results concisely․ Avoid jargon and ensure readability․ Highlight abnormal findings and correlate them with clinical implications․ Regularly review and update records to reflect patient progress․ Ensure all information is easily accessible for future reference and continuity of care․
10․2 Preparing a Comprehensive Assessment Report
Preparing a comprehensive assessment report involves organizing findings from patient history‚ physical exams‚ and diagnostic tests into a clear‚ structured document․ It should include subjective symptoms‚ objective data‚ and interpretations‚ ensuring clarity and accuracy․ The report must highlight key abnormalities‚ diagnostic impressions‚ and recommendations for further management or referrals․ Using standardized formats and precise language enhances readability and ensures effective communication among healthcare providers․ This documentation serves as a critical reference for ongoing patient care and legal purposes․
Respiratory system assessment ensures accurate diagnosis and effective management of respiratory conditions․ It guides further testing‚ treatment‚ and patient monitoring to improve outcomes․
11․1 Summary of Key Findings
A comprehensive respiratory assessment integrates patient history‚ physical exam‚ and diagnostic tests to identify abnormalities․ Key findings often include symptoms like dyspnea‚ cough‚ or wheezing‚ alongside physical signs such as abnormal breath sounds or chest deformities․ Diagnostic tests like PFTs‚ imaging‚ or blood gas analysis provide objective data to confirm respiratory dysfunction․ These findings guide clinical decision-making‚ ensuring personalized care and effective management of respiratory conditions․ Accurate documentation of these results is essential for continuity of care and future reference․
11․2 Referral and Follow-Up Recommendations
Timely referrals to specialists‚ such as pulmonologists or thoracic surgeons‚ are crucial for patients with complex respiratory conditions․ Regular follow-ups should be scheduled to monitor symptom progression and treatment responses․ Patients with severe or chronic conditions may require ongoing care‚ including lifestyle modifications and medication adjustments․ Clear communication between healthcare providers ensures coordinated management․ Patient education on self-monitoring and adherence to treatment plans is essential for improving outcomes․ These steps ensure comprehensive‚ patient-centered care and optimal long-term respiratory health․